"Just as our soul, being air, holds us together, so do breath and air encompass the whole world." Anaximenes (585–528 BCE)
My Father’s Death
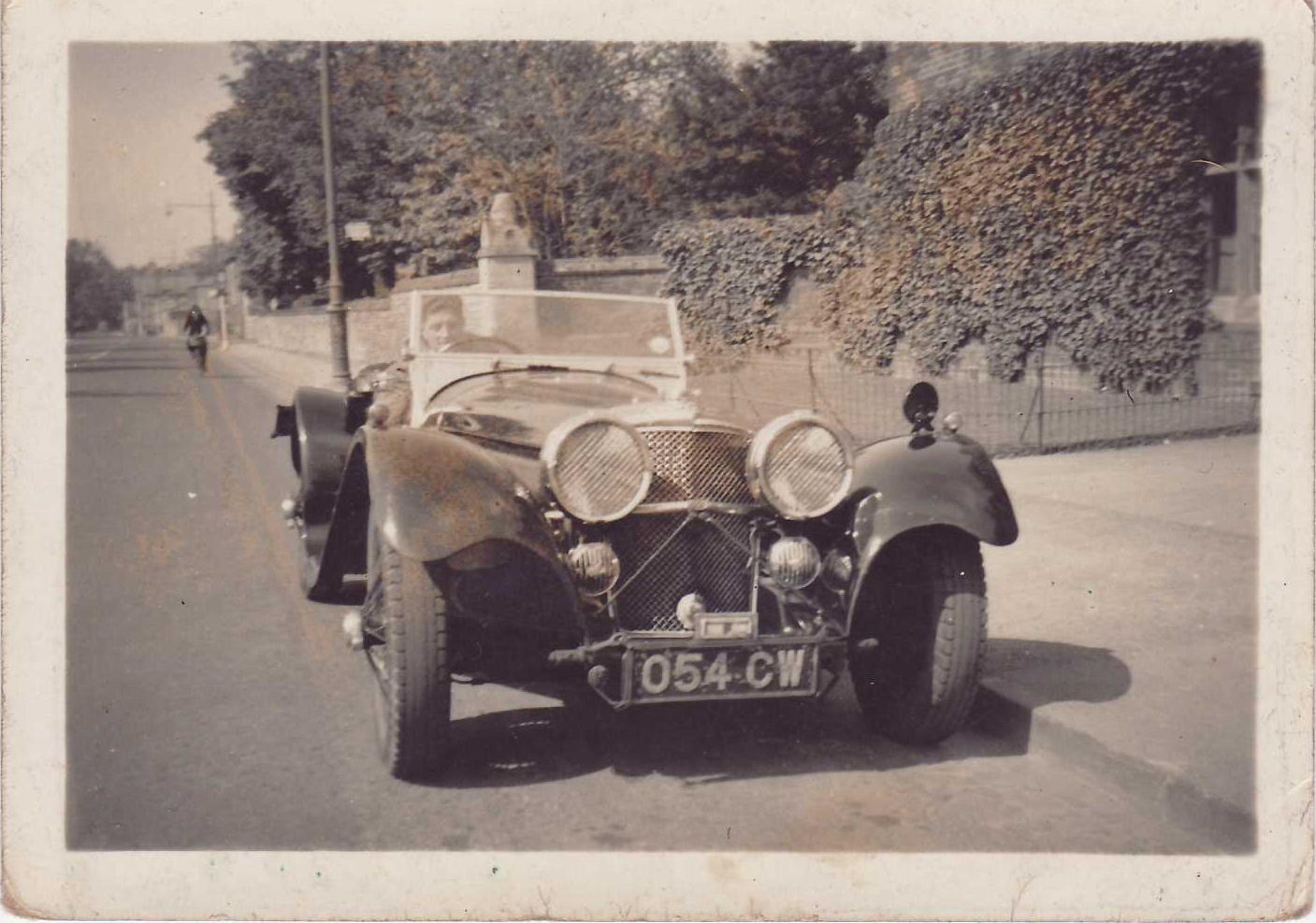
My father died from pancreatic cancer in 1970—he was just 54 and I was 21, raw and confused. At 23, he was called up to fight in World War II, and in 1941 was shipped off to Egypt to join the Eighth Army—the Desert Rats. He grew up in a poor household in Glasgow, Scotland, and took on the hard-bitten attitudes and hard-drinking lifestyle common amongst his peers. He had an enduring love of the sea. For the decade before his death he skippered a trawler and ran a shark fishing boat out of Newquay harbour in Cornwall, during the English postwar tourist boom. He loved the challenges of heavy weather fishing, quickly mastering boatmanship and its spin-offs: engine maintenance, knots, wrestling with tackle, repairing nets and crab pots, sculling dinghies, reading the weather, spotting shoals, and avoiding accidents with fish hooks and reeling hawser (although there were a few of those—attested by broken fingers and scars). To this day I have no idea whether or not he could swim—I certainly never saw him enter the water except to wade. But whatever the sea gave off, he drank it in and thrived on its tonic.
We only have so many breaths, so we must use them wisely.
When the cancer found purchase—it started in the pancreas and rapidly spread—he plummeted from feeling out of sorts to a heart-rending fragility. After a short period in hospital he was transferred home—thin, bed bound, often in extreme pain, and eventually drifting in and out of long periods of deep, opiate-induced sleep. From diagnosis to death was less than six months. On his deathbed he whispered confessional stories to me of his time in Egypt during the war—of smoking kif with Arabs; and of a party trick by a fellow platoon member of swallowing ground-up glass, bursting the myth that this acts as a poison. My father’s death rattle lasted twelve hours, an eerie gurgling sound, as if breathing through the mouth underwater.
When he was diagnosed with terminal cancer, both his family doctor and the consultant oncologist did not reveal the diagnosis to him. They took my mother, my brother, and me aside, told us the diagnosis and prognosis, and asked us to not divulge anything to him. They told my father that he had complications from an operation on his gallbladder (that is how the cancer was first discovered) that would clear up in time. I remember recoiling at the moral dilemma the doctors had set us—to not share the fatal diagnosis with my father but to spin a web of disguise through white lies—yet I joined the charade until the end. My dad, of course, knew that he was seriously ill, but the word "cancer" was never brought to the table. I was at his bedside when he drew his last breath. Laura Marks (2014) says: "Associated with the soul, animating the lungs, breath is that invisible and usually intangible entity that makes its passage known sonically": the hollow gurgling of the death rattle, then the sigh of resignation, and finally the wholesale withdrawal of noise—the void filled by the family’s collective sobs. Between the cry of birth and the just audible sigh of death, a life is measured in breaths, according to Buddhism. We only have so many breaths, so we must use them wisely.
I wrote this poem about my father’s death (Bleakley 2016):
My Father’s Atlantic Cure
Fishing with my father in a varnished
Boat fit for a coffin, decked with the Saltire –
His clenched hands blue and white too, with the cold,
Showing a keyboard of bruised knuckles.He died white and blue in his bed, limbs splayed,
A smudge on his mouth like beaten egg white,
A bluish body as slight as fish flakes
Crossing the longitude of the bedsheet.His storms had passed and their traces puddled –
A fisherman torn from his pots and nets
Belly up on a cold cotton island
In a dark room, with the smell of smoked fishLodged in the grain of the woollen carpet,
Whiskey breath’d, black-hair’d St Andrew, arms
And legs akimbo, pinned to the ceiling,
My father whispering:A vision! A vision!
A saltwater flood, the room swept away,
His heart stops, the catch is hauled in slowly.
There are beer and cigarettes at the funeral,
His body burned, we stain the day with salt tears.
Three things in particular struck me about his death: first, the obscene pact of secrecy that we set up with the doctors based around subscription to the stigma that cancer carried; second, the irrational tenacity that we, as a family, showed in sticking religiously to that pact; and third, the oncologist’s disturbing language register, describing the "invasion" of the cancer and how my dad had already "lost the war." I found the use of war metaphors particularly confusing because my father had no desire—or energy—to "fight" his illness. He was a combat veteran; he’d had his fill of war.
Medicine’s Inflation
In the years after my father’s death, I increasingly questioned what I saw as the deception of the doctors and our collusion with this deception, and felt palpable guilt about this. Later, I became aware of the seminal field study of Barney Glaser and Anselm Strauss (1967) that founded "grounded theory"—in which theory is built up from systematic analysis of data rather than data being collected to test a prior theory (Nathaniel and Andrews 2010). This study looked at how doctors and nurses in the 1960s interacted with people dying in hospitals from terminal illnesses, particularly cancers. Glaser and Strauss observed that it was common for doctors to enter into a pact with families in which patients were not told of their imminent demise, but were led to believe that they would recover. Cancer carried a huge stigma. Further, nurses were expected to talk with patients about their impending deaths only with the consent of physicians.
Medicine colonises the voices of patient and family.
This knot of deception—familiar from my father’s death—was termed a pact of "closed awareness." Nathaniel and Andrews (2010) described this pact as an "atmosphere of organized secrecy," where "family members purposely maintain the fiction that the dying patient might recover." Sadly, "This context does not allow patients to close their lives with proper rituals. Because of the organized deception, relatives’ grief cannot be expressed openly." In short, this particular posture of medical culture showed an extraordinary level of inflation—where doctors extend their legitimate specialist technical roles into questionable forms of imperialism and authoritarianism as they adopt particular communication strategies, in turn manipulating family members’ actions in diverting their natural concern and grief. In other words, the capital of emotional response and grief held within the family comes to be owned and distributed by the medical profession according to its whims, rather than an open and transparent ethical framework. Medicine colonises the voices of patient and family. This posture was prevalent in the mid to late 1960s, and times have changed. It is now common for those dying from cancer to be given their diagnosis and prognosis. However, while the specific culture that Glaser and Strauss explored may be seen as an historical anomaly, medicine’s inflations in general persist, as we shall see.
Cultures take on pomp, and egos inflate. In physics, inflation means swollen by air or gas; in economics, increase beyond proper limits; in psychology, puffed up with vanity, pride, or false notions—a state of mind characterized by an exaggerated sense of self-importance and need for admiration, compensated by feelings of inferiority. Read psychoanalytically, inflation is then a symptom of basic insecurity (fear of failure; intolerance of ambiguity). Medicine’s historical legacy of paternalistic, hierarchical, masculine heroism—preferring individualism to collaboration; opaque to the scrutiny of outsiders; refusing to own its multiple errors; and, at worse, arrogant and self-serving—advertises what psychoanalysts term "inflation of the ego," the basis of a Narcissistic Personality Disorder (NPD).
Contemporary illustrative examples of modern medicine’s inflation include its refusal of medical error, personal-confessional autoethnography, and overdetermined junior doctors on the road to burnout, discussed below.
Refusal of Medical Error
Estimates of how many people die from avoidable medical error in North America range from around 25,000 per annum (Shojania and Dixon-Woods 2017) to 250,000 (Makary and Daniel 2016). The former conservative estimate is probably closer to reality, as studies of medical error are riddled with methodological problems (Gianoli and Dunn 2016). My concern here, however, is not to enter the debate about the numbers. Rather, I am more interested in the almost hysterical intensity of response—effectively a denial—of certain doctors and surgeons to the higher estimate of medical error. The popular medical website Medscape (www.medscape.com/) hosted a summary of a widely critiqued study by Marty Makary (a surgeon) and his colleague, Michael Daniel (a healthcare research fellow). Published in the British Medical Journal in 2016, this article claimed that medical error in the United States is the third leading cause of death, with over 250,000 hospital-based deaths per annum, yet "medical error" does not appear as the cause of death on any certification.
Of the 500 readers’ responses to the article summary, nearly all from physicians, the majority showed sober skepticism, pointing out, for example, that many deaths resulting from surgical interventions on very ill or elderly patients disguise the fact that the patients would have died without the intervention. However, a significant minority offered heated outrage at the perceived inflation of the figures, disclosing their own inflations:
Among the words we can publish that were used to describe Makary and Daniel’s study findings were: "garbage," "tripe," "extrapolated hogwash," and "bogus." Still others described them as "outrageous," "absurd," "insulting," and "a joke." (Stokowski 2016)
However, in a second wave of comment under the heading "Doctors in Denial?", one pediatrician commented differently:
Medical errors are hard to accurately quantify. They are hugely underreported . . . people are practicing at the edge of their scope and not appropriately asking for guidance. Be careful of the ego and try to be aware of what you don’t know [my emphasis].
A nurse followed with the comment: "Instead of asking what we can do about this problem, most are variations on exclamations of denial." So, be careful of the ego; do not be in denial. Even if the numbers are adjusted down to a low estimate, there is still an evident problem with the incidence of medical error. Denial of the extent of this problem is a form of inflation.
Personal-Confessional Autoethnography
The contemporary genres of the personal-confessional autobiography and autoethnography from doctors and surgeons have burgeoned in recent years. Amongst the most successful of these, certainly in terms of book sales, are from the late American neurosurgeon, Paul Kalanithi (2016), and the recently retired British neurosurgeon, Henry Marsh (2014, 2017). Kalanithi writes of how he was driven to succeed in medicine to such an extent that it brought his marriage to the edge of ruin. He describes the punishing work schedules and harsh apprenticeship in learning brain surgery, the forming of a tough-minded arrogance as standard identity construction, and the impossibly high expectations of success, again driven by fear of failure and intolerance of ambiguity. Tragically, as Kalanithi confesses, his ego was tempered only by the rapidly encroaching shadow of his fatal lung cancer—a humbling by impending death at the beginning of what promised to be a glittering career.
Henry Marsh writes of a growing awareness only late in his career of his narcissism: "I often think I became a brain-surgeon to justify my own sense of self-importance." He warns that seeking out team members who will challenge and restrain you is essential to check medical hubris and egomania. Doctors shouldn’t work in isolation: "People working on their own get out of touch and it corrupts you . . . it’s hubris isn’t it? The funny thing about medical hubris is that nemesis is visited on the patients rather than the surgeon." That’s not a "funny thing," but sad and reprehensible.
Marsh seems to relish the reprehensible. In a recent interview in the UK’s Observer (Adams 2017), Marsh says that doctors and surgeons "have a very complicated relationship with patients . . . as soon as we have any interaction with patients, we start lying. We have to. There is nothing more frightening for a patient than an anxious or doubtful doctor." This is a good example of "old school" medical morality, one of double standards grounded in inflation.
Overdetermined Junior Doctors on the Road to Burnout
Confessions of a Junior Doctor, a 2017 UK television documentary, followed several junior doctors in their first months of residency at one UK hospital. They were, to a person, hardworking, sincere, and dedicated. But each, nevertheless, showed symptoms of inflation, infected by the culture of medicine. Their common "lite" form of inflation was overdeterminism—such as ordering too many tests or overdiagnosing—based on perfectionism and fear of failure. A knock-on effect, however, was working without due regard to their own health, leading to exhaustion and, in one case, to illness and burnout, thus compromising patient care and safety. Of course, this is a primary structural symptom of an underresourced National Health Service (NHS). However, doctors can also wear their exhaustion as a badge of honour.
A severely underweight young man is admitted to hospital. He had been admitted on four previous occasions, and the male junior doctor treating him saw on his notes that he had been tested for a number of potential disorders without anything irregular showing up. The knee jerk reaction of the junior doctor—failing to see the wood for the trees—was to order more tests. When these came back as negative, the resident was openly puzzled and decided to keep the young man in for observations. Nowhere in this episode, however, did the doctor seem to open up conversation with the patient that might have given context to the latter’s condition. Any experienced psychotherapist, clinical psychologist, or psychiatrist would have immediately suspected anorexia as a cause of the weight loss. The junior doctor was fixated on a physical rather than psychological cause.
Finally (on camera), the patient asked to speak to the doctor and told him that he had been eating only crisps for several days, and that he regularly did not eat for days on end. He confessed to smoking large amounts of cannabis every day. The inflation of the medical approach (overdetermined testing) had obscured the obvious: long-term episodes of cannabis use leading to loss of appetite and subsequent anorexia. Physical screening was unnecessary—the patient needed to eat and to entertain psychological therapy to get to the root of the cannabis addiction.
A second male junior doctor, patently a high achiever and intolerant of failure, was working on a neonatal unit and had to take blood from a premature baby. After three attempts, he failed to obtain the sample. An experienced nurse was in attendance and she took over, getting blood on the first try. Rather than asking the nurse for some tuition and guidance, the doctor simply chastised himself on camera for his lack of ability, ignoring potential learning from the nurse. As the French physician Claudina Michel-Teitelbaum (2016) suggests, medicine’s inflation is reproduced through education and socialisation:
In medical schools, students are trained to be highly confident in the power of medicine and are taught that there is a precise and effective procedure for every disease that has to be implemented. They are prepared to be heroes and to save lives. As heroes they are armed with potent weapons— . . . medical devices and sophisticated drugs . . . .
Putting Medicine on the Couch
Overall, medicine does an exceptional job under extreme pressure, but it also shoots itself in the foot unnecessarily. That medicine inflicts avoidable physical and psychological wounds on patients, colleagues, and doctors is clear, despite the Hippocratic injunction to "first, do no harm." Why this should be the case is unclear. Here, I suggest that inflation is a major root cause for such slippage, grounded in the culture’s refusal of democracy and authentic social justice, including gender equality, within its own ranks.
While some medical error arises from technical mistakes, the majority of such error is grounded in nontechnical, systemic processes of miscommunication, such as not following protocols and ineffective teamwork.
While some medical error arises from technical mistakes, the majority of such error is grounded in nontechnical, systemic processes of miscommunication, such as not following protocols and ineffective teamwork. The inability for some doctors to perform well in the context of nonhierarchical, interprofessional clinical teams rests again with an aspect of inflation—the masculine, heroic, and fiercely competitive impulse inviting individual responsibility, but refusing the formation of democratic habits.
This resistance to democratization and feminizing is itself grounded in an historical-cultural effect—the influence of two guiding metaphors that have shaped medical practice and values since the Enlightenment: the body as a machine and medicine as war, discussed below (Bleakley 2017). These didactic metaphors are, in turn, grounded in a wider historical-cultural effect: the "imagination of air" (Hillman 2014), or the "aerial imagination," characteristic of early Enlightenment values and practices, discussed later. I then move through three levels to explain medicine’s inflation: first, the refusal of democratization; second, that such refusal is grounded in the pervasive influence of two key metaphors; and third, that these metaphors in turn are grounded in the discourse of the Enlightenment’s scientific aerial imagination, the legacy of which remains potent.
Metaphor 1: The Body as Machine
Too often the consultant oncologist who diagnosed my father’s illness referred to him in terms of the cancer and the afflicted organ rather than the person, his suffering, and his sudden shrinking circle of life. Medicine’s inflation depends in part upon a parallel and compensatory deflation of patients, while reduction of the complexity of the body to a linear machine suggests intolerance of ambiguity.
Unfettered by the religious observation that prevented Galen (130–210) from dissecting humans, the Flemish doctor Andreas Vesalius (1514–64) dissected bodies of executed criminals provided by a sympathetic Paduan judge. Vesalius corrected fundamental errors in Galen’s work, stemming from extrapolating to the human from animal dissections. Vesalius reduced the body to a shell housing organs, described as the Fabrica—Latin for "something that is made," or a "machine." Vesalius then promoted a mechanical imagination of the body that has shaped medical culture to this day. Patients are reduced to their symptoms, where the body is a set of engineered components: for example, the brain has "wiring," the liver is the body’s "factory," and the kidneys are a "wastewater filter." Almost a century after Vesalius, the philosopher René Descartes (1596–1650), on the eve of the Enlightenment, said that "the body is to be regarded as a machine," an automaton. In the wake of Descartes, the celebrated Italian physician Giorgio Baglivi (1668–1706) extended the mechanical imagination of the body through finer grain analogies, where, for example, the stomach was compared to a flask, the teeth to scissors, blood vessels to pipes, and viscera and glands to sieves.
Metaphor 2: Medicine as War
I talked earlier of how I was puzzled when the oncologist who was treating my father described cancer as an "invading" force, a territorializing enemy. I agree with Susan Sontag’s (1978) analysis that the use of martial metaphors merely adds to the stigma already suffered by those with cancer—but Sontag goes too far when she demands that metaphors be eradicated from medical discourse altogether. Rather, we need to know why such metaphors are used—where they appeared historically and how they may already be "dead" or can—and should—be replaced by other, more helpful metaphors (Bleakley 2017).
In the Medieval to Early Modern period, my father’s cancer would have been ascribed to an imbalance of humours or an excess of vital forces. Illnesses "lay" on people (passive language) rather than "attacking" them (active language). Hippocrates (c.460–370 BCE) first named observable tumours "cancer"—Greek karkinos, Latin carcinos—after the crab and crayfish, analogous with the sideways creep of tumours ("metastasis" means "change of position"). The disease was imagined as "shifty," scuttling sideways, but not as "aggressive."
The martial language of aggressive tumours, and aggressive treatments to combat them, can be traced to the English poet and cleric John Donne’s (1573–1631) 1627 sermon: “Devotions Upon Emergent Occasions.” Donne describes his illness in 1627 as resembling a "siege" and "cannon shot."
The martial language of aggressive tumours, and aggressive treatments to combat them, can be traced to the English poet and cleric John Donne’s (1573–1631) 1627 sermon: “Devotions Upon Emergent Occasions.” Donne describes his illness in 1627 as resembling a "siege" and "cannon shot." He thought he was dying from a fever "that blows up the heart," also describing an "illness that invades." But it was the celebrated English physician Thomas Sydenham (1624–89) who fully embraced militaristic metaphors and created the metaphorical climate that has shaped modern medicine, still in full flow today with personalized drug regimes "targeting" genetic faults and the ongoing "war on cancer."
Sydenham’s language is Homeric: "I attack the enemy within," where: "A murderous array of disease has to be fought against, and the battle is not a battle for the sluggard . . . I steadily investigate the disease, I comprehend its character, and I proceed straight ahead, and in full confidence, towards its annihilation." Medicine is not for the fainthearted, but a full-blooded battle reinforcing the dominance of the heroic male. No room for dithering here, but "proceed straight ahead" in full certainty.
By the nineteenth century, Louis Pasteur (1822–95) was using the same active militaristic language, describing invading armies laying siege to the body that becomes a battlefield. A "war against cancer" was first described in a lead article in the British Medical Journal in 1904. The "fight against cancer" was likened to imperialist domination, the disease described as "darkest Africa" waiting to be discovered and conquered. Later, cancer cells were identified with Bolsheviks as "anarchic," threatening the stability of the body. Richard Nixon declared a full-scale "war on cancer" in signing the National Cancer Act of 1971, launching a $1.6 billion "federal crusade" to "conquer" cancer, using the most "aggressive" treatments to beat the "invading, killer cells."
In 2011, the 1989 Nobel Prize-winning Director of the National Cancer Institute (NCI), Dr. Harold Varmus, was asked at a conference: "Can you give us an overall sense of what we may have accomplished over the last four decades?" Varmus replied: "It’s inaccurate, in my view, to think of a war on cancer as though cancer were a single, individual enemy, nor is the metaphor of war exactly right." Corpus linguistic analysis (Semino et al. 2017) shows that in cancer discourse, patients commonly resort to violence and war metaphors. Yet research shows that cancer patients who view their disease as an "enemy" show higher levels of anxiety and depression, a poorer quality of life, higher levels of pain, and less ability to cope overall than those who represent their illness with a different meaning (Bleakley 2017). It is likely that patients use war metaphors unthinkingly. Many do not subscribe to this metaphor complex, but use other nonmartial metaphors such as cancer as a "journey."
Following the poet Wallace Stevens, who said, "The world is presence, not force," we might replace martial medicine with a more feminine, collaborative, and tender approach.
Following the poet Wallace Stevens, who said, "The world is presence, not force," we might replace martial medicine with a more feminine, collaborative, and tender approach. For example, "hospital" has the same root as "hospitality." Such a lyrical medicine offers an alternative to the standard epic, tragic, and dark comic genres of practice (medicine has developed an unsavoury black humour at patients’ expense (Piemonte 2015).
The Aerial Imagination
The checks and balances that control potential inflation in a democracy, whether in persons or economies, arise from tolerant, collaborative engagement. Where the heroic imagination and a certain level of intolerance continue to feed medicine, there is no check on inflation. Machine and martial metaphors, however, offer necessary but not sufficient explanations for medicine’s inflation. We must also explore what gives these didactic metaphors such impetus and stamina. My suggestion is the legacy of the Enlightenment’s aerial imagination. This imagination inflates science beyond its boundaries of an explanatory and exploratory framework to one of imperialism, including domination and control of nature, and in medicine (often in good faith), domination and control of patients’ experiences.
Of the realms of nature that might be controlled, the very air we breathe is the most obvious (Kean 2017). This intangible air must first be made tangible through close examination—dissected, measured, weighed—subsequently conquered (human flight), finally controlled (e.g., through mass production of soda waters), and made subject to ownership (capitalism’s influence upon air quality and access to clean air). James Hillman (2014) describes the rise of a scientific "imagination of air" in terms of the collapse of a Medieval/ Renaissance worldview—that of alchemy. When a metal is burned to an ash (calcination) and the residue is weighed, it weighs more than the original metal. The alchemists ascribed this to calcination driving off a substance— phlogiston—that animated the material (think Ariel in Shakespeare’s The Tempest). Where phlogiston is released, the loss of enervating spirit (the Greek pneuma: breath or in-spiration) results in heaviness. It took a group of experimental chemists in the 1770s to reject this speculative alchemy, showing that roasted metals gain weight because oxygen is added. One of these chemists, Joseph Priestley, recorded that pumping oxygen into a container with a candle made the flame brighter, and into an enclosed area with mice made the mice livelier, while inhaling pure oxygen led to an exhilarating effect that Priestley suggested might become a popular indulgence. Oxygen inflates.
Where the heroic imagination and a certain level of intolerance continue to feed medicine, there is no check on inflation.
Priestley, however, would never see "airs" as capital subject to ownership and unfair redistribution, a later phenomenon accelerated by the Industrial Revolution and the spread of air pollution. His house in England was burned down because of his dissent from the orthodoxy of the Church and associated authoritarian politics of the time, and he fled to America, where he sought a more democratic climate. Ironically, Priestley discovered how to carbonate water (the basis of sodas) in 1767, thus paving the way for the production of Coca Cola just over a century later. Now, two billion bottles a day are drunk worldwide and Coke has become a symbol of the unacceptable face of commercialism, capitalism, and imperialism, the very forces that Priestley despised.
The aerial imagination also materialised through conquering not only the air—the Montgolfier Brothers launched the first hot air balloon flight in 1783—but also the dark. Gas lighting was perfected in 1800, and by 1820 Birmingham, London, Preston, Paris, Vienna, Baltimore, and Philadelphia had extensive street lighting, advertising the democratic potential of the new "airs."
Combat Breathing and the Survival of the Sickest
The Afro-Caribbean psychiatrist and revolutionary Frantz Fanon described the "combat breathing" of Algerian prisoners of war as a form of resistance in the presence of their French colonist oppressors. This breathing is a literal in-spiration, a collective deep breath to restore energy for acts of resistance: "breathe in, hold, count to four; breathe in, hold, count to four . . . ," and so on. "Combat" is used here ironically, for combat breathing is an act of passive resistance, as occupation changes the atmosphere of a culture ("you can observe my breathing, but you cannot occupy my breath"). Fanon (1959) wrote:
There is not occupation of territory, on the one hand, and independence of persons on the other. It is the country as a whole, its history, its daily pulsation that are contested, disfigured, in the hope of a final destruction. Under these conditions, the individual’s breathing is an observed, an occupied breathing. It is a combat breathing.
Sharing an atmosphere involving medical intervention means that the patient can be deprived of breathing space as his or her territory becomes occupied. In my father’s case, the whole family was occupied as we colluded with the doctors, thus letting slip the opportunity to adopt combat breathing, or what Homi Bhabha (2004) calls "sly civility" —tactics of resistance that appear to offer conformity with, but subtly undermine, the colonizer’s presence: a version of Thoreau’s and Gandhi’s "civil disobedience."
I have described three cures for medicine’s inflation: (1) democratizing and feminizing medicine; (2) shifting the didactic metaphors that shape medicine and medical practice; and (3) deflating the imperialistic aerial imagination. In this section, I describe a fourth cure: to undermine medicine’s tacit subscription to Utilitarianism, defined as "the doctrine that an action is right in so far as it promotes happiness, and that the greatest happiness of the greatest number should be the guiding principle of conduct" (OED). But one person’s "happiness" (and "health") is another’s misery, and the birth lottery leaves many with disabilities and disadvantages where "health" becomes a relative notion. Further, even the very healthy may risk their lives through challenging sports or lifestyles. One key aspect of medicine’s inflation, also a tactic for both legitimate and illegitimate occupation of the patient’s atmosphere, is to make distinctions between the "normal" and the "pathological" that are, in fact, arbitrary (Canguilhem 1991).
Medicine can democratize (and deflate) under its own steam by challenging long-held subscription to ideals of health, embracing the paradoxical value of sickness and suffering.
Medicine can democratize (and deflate) under its own steam by challenging long-held subscription to ideals of health, embracing the paradoxical value of sickness and suffering. The performance artist and academic Martin O’Brien (2017) describes a "survival of the sickest," challenging pieties based on holding untenable distinctions between health and sickness. O’Brien, in an act of sly civility, reverses Darwin’s "survival of the fittest" by imagining a "Zombie Apocalypse" where: "I’d eat you to stay alive. I wouldn’t even think twice. . . .It’s survival of the sickest! If it were the zombie apocalypse, only the infected could survive."
Martin O’Brien has cystic fibrosis (CF), so his breathing works against the grain, as his lungs fill with fluid. This condition leads to an early death—the average life expectancy for someone with CF is currently 37 years. He needs regular physiotherapy for airway clearance, to free up mucus that would otherwise drown him. But O’Brien has turned his illness and impending death into a paradoxical gift by developing a radical durational performance art around his symptoms and consequent lifestyle (http://www.martinobrienperformance.com). Here, combat breathing is every day and therapeutic—an act of resistance against colonizing by straight cultural values and standard medical approaches. O’Brien’s work advertises Nietzsche’s claim that artists can be diagnosticians of culture, challenging cultural norms. He takes the theme of the zombie—the living dead—as an image for the "survival of the sickest" that directly challenges the traditions of the aerial imagination and its inflations, within which conventional modern medicine has been cocooned for three centuries. O’Brien’s performance interventions bring medicine down to earth with a bump, puncturing its pieties.
Coda: The Valve and Medical Education
In this Humanities Futures "think piece" paper, I have tracked some key historical conditions of possibility for the emergence of modern medicine’s primary symptom: inflation. I have also discussed how such inflation may be treated. While in danger of employing the very material imagination I critiqued earlier, a useful metaphor for "tuning" medicine’s inflations is the valve. Such control is the main purpose of medical education. It is through curriculum innovations in medical education that medicine’s inflation is best treated: through democratizing and feminizing medicine (also addressing avoidable medical error); embracing more productive shaping metaphors than the mechanical and martial; and deflating the long tradition of the imperialistic aerial imagination and subscription to Utilitarianism (ideals of health and well-being) through adaptive combat breathing.
In the opening section of his novel Against the Day (2006), Thomas Pynchon imitates the genre of the adventure comic, describing an intrepid crew of hydrogen balloonists, the "Chums of Chance," who are making their way to Chicago for the World’s Fair in 1893 in their surveillance balloon "Inconvenience":
. . .the well-meaning but far from dextrous Miles Blundell had somehow contrived to wrap the pull-rope leading to the valve mechanism around his foot, and could be seen moving that extremity to and fro . . . in hopes that the spring-loaded valve would thus, somehow, close again—for it had already allowed an enormous quantity of hydrogen gas to escape the envelope in a sudden rush, causing the ship to plummet toward the lakeside like a toy dropped by some cosmic urchin.
Let us then take this scene of the (mis)control of the balloon’s valve as a metaphor for the tempering of the ego—of individuals, but more importantly of a culture. I acknowledge again that, like the fictional Miles Blundell, medicine too is "well-meaning," but perhaps far from dextrous when it comes to critical reflexivity—close scrutiny of its own ingrained traditions, values, and habits. Where too much hot air is allowed in because of poor control of the valve, the balloon becomes inflated and sails off, untethered. Where air is allowed to escape suddenly (deflation or a puncturing of the inflated ego), there is a plummeting, and potential crash. The inflated ego is liable to plummet from great heights, an Icarus figure, prefiguring burnout (Peterkin and Bleakley 2017).
Where, in nature, symptom and cure are often side by side (the burning desert sun and the aloe vera cactus; the stinging nettle and the dock leaf), so in medical culture the arrogant doctor or surgeon who sneers at contemporary medical education sits side by side with the medical education enthusiast. The latter’s patient listening and responses may slowly cure the inflation of the former, acting as a valve mechanism encouraging deflation, a condition also of humility.
Resistance to hegemony by an inflated medicine is offered by a humble, patient-centered, collaborative, and tender medicine softening and subverting the phallogocentric medical gaze. Franz Fanon’s combat breathing refers also to the disguised breathing of Algerian women donning the veil (which the French sought to ban) in resisting French colonialism in North Africa. In donning the veil, the breath of resistance was amplified as the women frustrated the direct gaze of the oppressors seeking control. This scenario can act as both parable and metaphor for resistance to the colonizing medical gaze shadowed by the apocalyptic "survival of the sickest."
References
Adams, Tim. 2017. "Henry Marsh: ‘The Mind-Matter Problem Is Not a Problem for Me – Mind Is Matter.’" Interview with Henry Marsh. The Observer, July 16. https://www.theguardian.com/science/2017/jul/16/henry-marsh-mind-matter-not-a-problem-interview-neurosurgeon-admissions.
Bhabha, Homi. 2004. The Location of Culture. 2nd ed. London: Routledge.
Bleakley, Alan. 2016. Hook, Line, & Sinker & Other Poems. Dartington: Acts of Language.
___. 2017. Thinking with Metaphors in Medicine: The State of the Art. London: Routledge.
Canguilhem, Georges. 1991. The Normal and the Pathological. New York: Zone Books.
Fanon, Frantz. 1959. A Dying Colonialism. New York: Grove Press.
Gianoli, Gerard J., and John Dale Dunn. 2016. "Unreliable Research on Error-Related Hospital Deaths in America." Journal of American Physicians and Surgeons 21: 104–08. Accessed July 19, 2017. http://www.jpands.org/vol21no4/gianoli.pdf.
Glaser, Barney, and Anselm Strauss. 1967. Awareness of Dying. New York: Aldine Publishing Company.
Hillman, James. 2014. "The Imagination of Air and the Collapse of Alchemy." In The Uniform Edition of the Writings of James Hillman. Vol. 5, edited by James Hillman, 263–315. Dallas, TX: Dallas Institute Publications.
Kalanithi, Paul. 2016. When Breath Becomes Air. London: Bodley Head.
Kean, Sam. 2017. Caesar’s Last Breath: The Epic Story of the Air Around Us. New York: Doubleday.
Makary, Martin A., and Michael Daniel. 2016. "Medical Error—The Third Leading Cause of Death in the US." British Medical Journal 353: i2139.
Marks, Laura U. 2014. Book Cover Commentary for Davina Quinlivan, The Place of Breath in Cinema. Edinburgh: Edinburgh University Press.
Marsh, Henry. 2014. Do No Harm: Stories of Life, Death and Brain Surgery. London: Weidenfeld & Nicholson.
___. 2017. Admissions: A Life in Brain Surgery. London: Weidenfeld and Nicholson.
Michal-Teitelbaum, Claudina A. 2016. "The Medical Bubble and the Opportunity to Harm." British Medical Journal 353: i2139. Accessed July 9, 2017. http://www.bmj.com/content/353/bmj.i2139/rr-56.
Nathaniel, Alvita K., and Tom Andrews. 2010. "The Modifiability of Grounded Theory." Grounded Theory Review 9 (1). Accessed July 9, 2017. http://groundedtheoryreview.com/2010/04/06/751/.
O’Brien, Martin. 2017. "If It Were the Apocalypse I’d Eat You to Stay Alive." Accessed July 9, 2017. http://www.inbetweentime.co.uk/wp-content/uploads/2016/10/MC_IBT_ProgNotes_MartinOBrien_070217_v01_Web.pdf.
Peterkin, Allan, and Alan Bleakley. 2017. Staying Human During the Foundation Programme and Beyond. Boca Raton, FL: CRC Press.
Piemonte, Nicole. 2015. "Last Laugh: Gallows Humor and Medical Education." Journal of Medical Humanities 36: 375–90.
Pynchon, Thomas. 2006. Against the Day. London: Jonathan Cape.
Semino Elena, Zsófia Demjén, Jane Demmen, Veronika Koller, Sheila Payne, Andrew Hardie, and Paul Rayson. 2017. "The Online Use of Violence and Journey Metaphors by Patients with Cancer, as Compared with Health Professionals: A Mixed Methods Study." BMJ Supportive & Palliative Care 7 (1): 60–66.
Shojania, Kaveh G., and Mary Dixon-Woods. 2017. "Estimating Deaths Due to Medical Error: The Ongoing Controversy and Why It Matters." BMJ Quality and Safety 26: 423–28.
Sontag, Susan. 1978. Illness as Metaphor. New York: Farrar, Strauss & Giroux.
Stokowski, Laura A. 2016. "Who Believes That Medical Error Is the Third Leading Cause of Hospital Deaths?" Medscape, May 26. Accessed July 7, 2017. http://www.medscape.com/viewarticle/863788.
This work is licensed under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.